SÁCH DỊCH “Y HỌC CHU PHẪU: QUẢN LÝ HƯỚNG ĐẾN KẾT QUẢ, ẤN BẢN THỨ 2”
Được dịch và chuyển thể sang tiếng Việt từ sách gốc “Perioperative Medicine: Managing for Outcome, 2nd Edition”
Dịch và chú giải: Ths.Bs. Lê Đình Sáng – Hiệu đính: Ts.Bs.Lê Nhật Huy
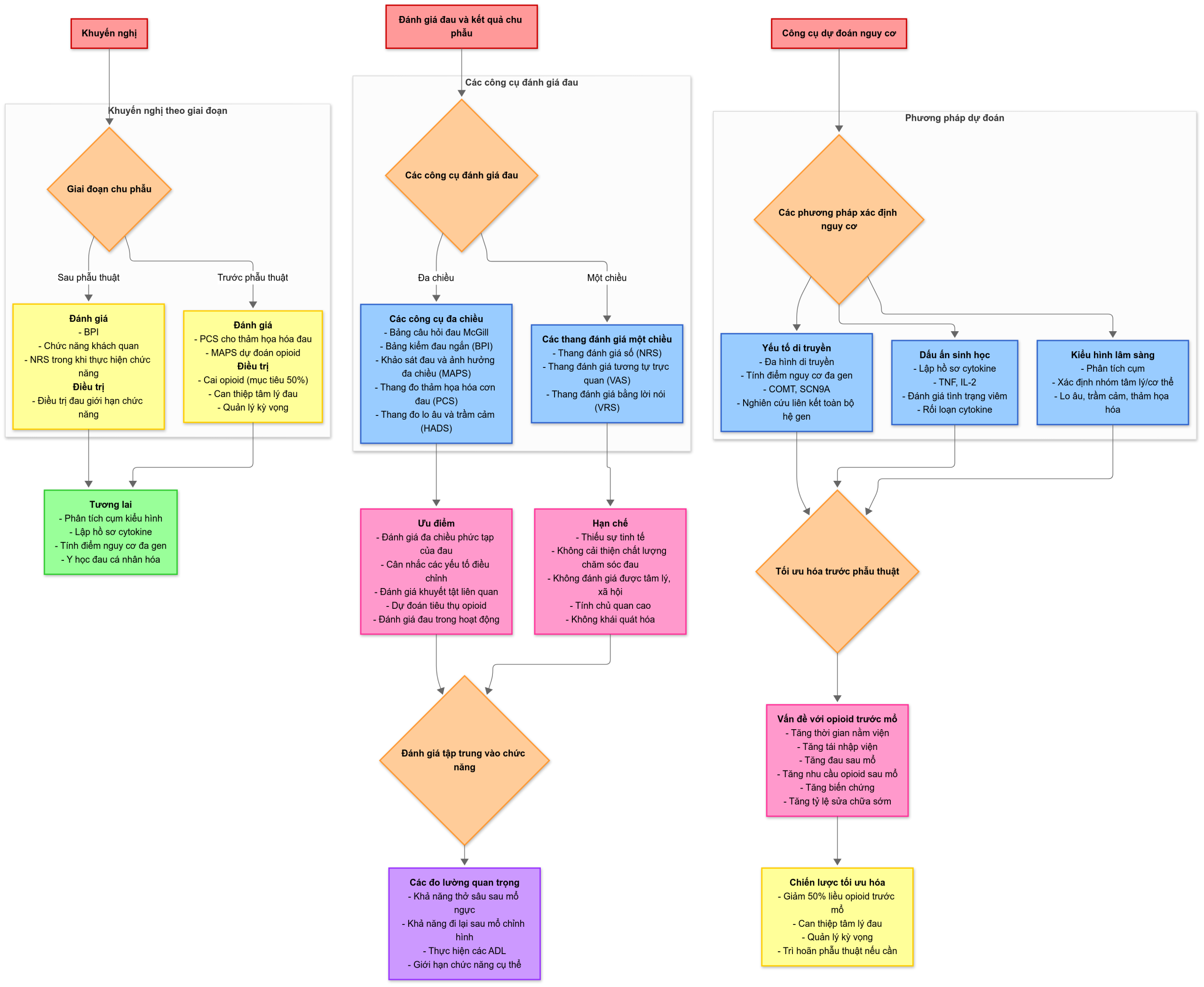
Chương 41. Cải thiện đau và kết quả điều trị trong giai đoạn chu phẫu
Improving Pain and Outcomes in the Perioperative Setting – Neil Ray and Thomas Buchheit
Perioperative Medicine, 41, 607-612
TÀI LIỆU THAM KHẢO
- Quality improvement guidelines for the treatment of acute pain and cancer pain: American Pain Society Quality of Care Committee. JAMA 1995; 274: pp. 1874-1880.
- Society A.P.: Principles of Analgesic Use in the Treatment of Acute Pain and Cancer Pain.2nd ed1992.American Pain SocietySkokie, Ill
- Health V.’.: Administration Memorandum: Pain as the Fifth Vital Sign. J Am Optom Assoc 1999; 70: pp. 619-620.
- Kolodny A., Courtwright D.T., Hwang C.S., et. al.: The prescription opioid and heroin crisis: A public health approach to an epidemic of addiction. Annu Rev Public Health 2015; 36: pp. 559-574.
- Helfand M., Freeman M.: Assessment and management of acute pain in adult medical inpatients: A systematic review. Pain Med 2009; 10: pp. 1183-1199.
- Breivik E.K., Bjornsson G.A., Skovlund E.: A comparison of pain rating scales by sampling from clinical trial data. Clin J Pain 2000; 16: pp. 22-28.
- Jensen M.P., Chen C., Brugger A.M.: Postsurgical pain outcome assessment. Pain 2002; 99: pp. 101-109.
- Brunelli C., Zecca E., Martini C., et. al.: Comparison of numerical and verbal rating scales to measure pain exacerbations in patients with chronic cancer pain. Health Qual Life Outcomes 2010; 8: pp. 42.
- Breivik H., Borchgrevink P.C., Allen S.M., et. al.: Assessment of pain. Br J Anaesth. 2008; 101: pp. 17-24.
- Mularski R.A., White-Chu F., Overbay D., et. al.: Measuring pain as the 5th vital sign does not improve quality of pain management. J Gen Intern Med 2006; 21: pp. 607-612.
- Kerns R.D., Jacob M.C.: Assessment of the psychosocial context of the experience of chronic pain.Turk D.C.Melzack R.Handbook of Pain Assessment.1992.Guilford PressNew York, NY, US:pp. 235-253.
- Krebs E., Carey T., Weinberger M.: Accuracy of the pain numeric rating scale as a screening test in primary care. J Gen Intern Med 2007; 22: pp. 1453-1458.
- Lowe N.K., Walker S.N., McCallum R.C.: Confirming the theoretical structure of the McGill Pain Questionnaire in acute clinical pain. Pain 1991; 46: pp. 53-60.
- Mendoza T.R., Chen C., Brugger A., et. al.: The utility and validity of the modified brief pain inventory in a multiple-dose postoperative analgesic trial. Clin J Pain 2004; 20: pp. 357-362.
- Yang J.C., Clark W.C., Tsui S.L., et. al.: Preoperative Multidimensional Affect and Pain Survey (MAPS) scores predict postcolectomy analgesia requirement. Clin J Pain 2000; 16: pp. 314-320.
- Granot M., Ferber S.G.: The roles of pain catastrophizing and anxiety in the prediction of postoperative pain intensity: A prospective study. Clin J Pain 2005; 21: pp. 439-445.
- Khan R.S., Skapinakis P., Ahmed K., et. al.: The association between preoperative pain catastrophizing and postoperative pain intensity in cardiac surgery patients. Pain Med 2012; 13: pp. 820-827.
- Papaioannou M., Skapinakis P., Damigos D., et. al.: The role of catastrophizing in the prediction of postoperative pain. Pain Med 2009; 10: pp. 1452-1459.
- Asmundson G.J., Katz J.: Understanding the co-occurrence of anxiety disorders and chronic pain: State-of-the-art. Depress Anxiety 2009; 26: pp. 888-901.
- Chou R., Shekelle P.: Will this patient develop persistent disabling low back pain?. JAMA 2010; 303: pp. 1295-1302.
- Guyatt G.H., Townsend M., Berman L.B., et. al.: A comparison of likert and visual analogue scales for measuring change in function. J Chronic Dis 1987; 40: pp. 1129-1133.
- Bendinger T., Plunkett N.: Measurement in Pain Medicine. Br J Anaesth Edu 2016; 16: pp. 310-315.
- Jamison R.N., Ross E.L., Michna E., et. al.: Substance misuse treatment for high-risk chronic pain patients on opioid therapy: A randomized trial. Pain 2010; 150: pp. 390-400.
- Prakken S, Buchheit T, Westover J, et al: Cost Savings Associated with Intensive Outpatient Pain Management of Duke Health System High Utilizers.
- Martinez V., Üçeyler N., Ben Ammar S., et. al.: Clinical, histological, and biochemical predictors of postsurgical neuropathic pain. Pain 2015; 156: pp. 2390-2398.
- VanDenKerkhof E.G., Hopman W.M., Goldstein D.H., et. al.: Impact of perioperative pain intensity, pain qualities, and opioid use on chronic pain after surgery. Reg Anesth Pain Med 2012; 37: pp. 19-27.
- Ondeck N.T., Bohl D.D., Bovonratwet P., et. al.: Discriminative ability of commonly used indices to predict adverse outcomes after poster lumbar fusion: A comparison of demographics, ASA, the modified Charlson Comorbidity Index, and the modified Frailty Index. Spine J 2017; 18: pp. 44-52.
- Larson K.J., Hamlin R.J., Sprung J., et. al.: Associations between Charlson Comorbidity Index and surgical risk severity and the surgical outcomes in advanced-age patients. Am Surg 2014; 80: pp. 555-560.
- Burgess J.R., Smith B., Britt R., et. al.: Predicting postoperative complications for acute care surgery patients using the ACS NSQIP surgical risk calculator. Am Surg 2017; 83: pp. 733-738.
- Fleisher L.A., Fleischmann K.E., Auerbach A.D., et. al.: 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2014; 130: pp. e278-e333.
- Jacob K.A., Hjortnaes J., Kranenburg G., et. al.: Mortality after cardiac surgery in patients with liver cirrhosis classified by the Child-Pugh score. Interact CardioVasc Thorac Surg 2015; 20: pp. 520-530.
- Brown J.R., MacKenzie T.A., Maddox T.M., et. al.: Acute Kidney Injury Risk Prediction in Patients Undergoing Coronary Angiography in a National Veterans Health Administration Cohort With External Validation. J Am Heart Assoc 2015; 4:
- Theunissen M., Peters M.L., Bruce J., et. al.: Preoperative anxiety and catastrophizing: A systematic review and meta-analysis of the association with chronic postsurgical pain. Clin J Pain 2012; 28: pp. 819-841.
- Tasmuth T., Estlanderb A.M., Kalso E.: Effect of present pain and mood on the memory of past postoperative pain in women treated surgically for breast cancer. Pain 1996; 68: pp. 343-347.
- Sullivan M., Tanzer M., Stanish W., et. al.: Psychological determinants of problematic outcomes following Total Knee Arthroplasty. Pain 2009; 143: pp. 123-129.
- Taenzer PMRJM : Influence of psychological factors on postoperative pain, mood and analgesic requirements. Pain 1986; 24: pp. 331-342.
- Yarnitsky D., Crispel Y., Eisenberg E., et. al.: Prediction of chronic post-operative pain: Pre-operative DNIC testing identifies patients at risk. Pain 2008; 138: pp. 22-28.
- Belfer I., Schreiber K.L., Shaffer J.R., et. al.: Persistent postmastectomy pain in breast cancer survivors: Analysis of clinical, demographic, and psychosocial factors. J Pain 2013; 14: pp. 1185-1195.
- Dworkin R.H., Turk D.C., Farrar J.T., et. al.: Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain 2005; 113: pp. 9-19.
- Cramer P., Hallek M.: Hematological cancer in 2011: New therapeutic targets and treatment strategies. Nat Rev Clin Oncol 2012; 9: pp. 72-74.
- de Jong T.D., Vosslamber S., Verweij C.L.: Moving towards personalized medicine in rheumatoid arthritis. Arthritis Res Ther 2014; 16: pp. 110.
- Hehn Von C.A., Baron R., Woolf C.J.: Deconstructing the neuropathic pain phenotype to reveal neural mechanisms. Neuron 2012; 73: pp. 638-652.
- Vollert J., Maier C., Attal N., et. al.: Stratifying patients with peripheral neuropathic pain based on sensory profiles: Algorithm and sample size recommendations. Pain 2017; 158: pp. 1446-1455.
- Harden R.N., Oaklander A.L., Burton A.W., et. al.: Complex regional pain syndrome: Practical diagnostic and treatment guidelines, 4th edition. Pain Med 2013; 14: pp. 180-229.
- Cruccu G., Sommer C., Anand P., et. al.: EFNS guidelines on neuropathic pain assessment: Revised 2009. Eur J Neurol 2010; 17: pp. 1010-1018.
- Demant D.T., Lund K., Finnerup N.B., et. al.: Pain relief with lidocaine 5% patch in localized peripheral neuropathic pain in relation to pain phenotype: A randomised, double-blind, and placebo-controlled, phenotype panel study. Pain 2015; 156: pp. 2234-2244.
- Demant D.T., Lund K., Vollert J., et. al.: The effect of oxcarbazepine in peripheral neuropathic pain depends on pain phenotype: A randomised, double-blind, placebo-controlled phenotype-stratified study. Pain 2014; 155: pp. 2263-2273.
- Maixner W., Diatchenko L., Dubner R., et. al.: Orofacial pain prospective evaluation and risk assessment study–the OPPERA study. J Pain 2011; 12: pp. T4-T11. e1-e2 https://doi.org/10.1016/j.jpain.2011.08.002
- Bair E., Gaynor S., Slade G.D., et. al.: Identification of clusters of individuals relevant to temporomandibular disorders and other chronic pain conditions: The OPPERA study. Pain 2016; 157: pp. 1266-1278.
- Schuler G.D., Boguski M.S., Stewart E.A., et. al.: A gene map of the human genome. Science 1996; 274: pp. 540-546.
- Yuan R., Zhang X., Deng Q., et. al.: Two novel SCN9A gene heterozygous mutations may cause partial deletion of pain perception. Pain Med 2011; 12: pp. 1510-1514.
- Zubieta J.K., Heitzeg M.M., Smith Y.R., et. al.: COMT val158met genotype affects mu-opioid neurotransmitter responses to a pain stressor. Science 2003; 299: pp. 1240-1243.
- Young E.E., Lariviere W.R., Belfer I.: Genetic basis of pain variability: Recent advances. J Med Genet 2011; 49: pp. 1-9.
- Kim H., Dionne R.A.: Individualized pain medicine. Drug Discov Today Ther Strateg 2009; 6: pp. 83-87.
- Diatchenko L., Slade G.D., Nackley A.G., et. al.: Genetic basis for individual variations in pain perception and the development of a chronic pain condition. Hum Mol Genet 2005; 14: pp. 135-143.
- Perera R.S., Dissanayake P.H., Senarath U., et. al.: Single Nucleotide Variants of Candidate Genes in Aggrecan Metabolic Pathway Are Associated with Lumbar Disc Degeneration and Modic Changes. PLoS ONE 2017; 12:
- Muralidharan A., Smith M.T.: Pain, analgesia and genetics. J Pharm Pharmacol 2011; 63: pp. 1387-1400.
- Bjorland S., Røe C., Moen A., et. al.: Genetic predictors of recovery in low back and lumbar radicular pain. Pain 2017; 158: pp. 1456-1460.
- Kehlet H., Jensen T.S., Woolf C.J.: Persistent postsurgical pain: Risk factors and prevention. Lancet 2006; 367: pp. 1618-1625.
- Nassar M.A., Stirling L.C., Forlani G., et. al.: Nociceptor-specific gene deletion reveals a major role for Nav1.7 (PN1) in acute and inflammatory pain. Proc Natl Acad Sci U S A 2004; 101: pp. 12706-12711.
- Reimann F., Cox J.J., Belfer I., et. al.: Pain perception is altered by a nucleotide polymorphism in SCN9A. Proc Natl Acad Sci U S A 2010; 107: pp. 5148-5153.
- Dib-Hajj S.D., Yang Y., Waxman S.G.: Genetics and molecular pathophysiology of Na(v)1.7-related pain syndromes. Adv Genet 2008; 63: pp. 85-110.
- Easton D.F., Pooley K.A., Dunning A.M., et. al.: Genome-wide association study identifies novel breast cancer susceptibility loci. Nature 2007; 447: pp. 1087-1093.
- Sladek R., Rocheleau G., Rung J., et. al.: A genome-wide association study identifies novel risk loci for type 2 diabetes. Nature 2007; 445: pp. 881-885.
- Clarke A.J., Cooper D.N.: GWAS: Heritability missing in action?. Eur J Hum Genet 2010; 18: pp. 859-861.
- Montes A., Roca G., Sabate S., et. al.: Genetic and Clinical Factors Associated with Chronic Postsurgical Pain after Hernia Repair, Hysterectomy, and Thoracotomy: A Two-year Multicenter Cohort Study. Anesthesiology 2015; 122: pp. 1123-1141.
- Agerbo E., Sullivan P.F., Vilhjálmsson B.J., et. al.: Polygenic Risk Score, Parental Socioeconomic Status, Family History of Psychiatric Disorders, and the Risk for Schizophrenia: A Danish Population-Based Study and Meta-analysis. JAMA Psychiatry 2015; 72: pp. 635-641.
- Ji R.-R., Xu Z.-Z., Gao Y.-J.: Emerging targets in neuroinflammation-driven chronic pain. Nat Rev Drug Discov 2014; 13: pp. 533-548.
- Radojčić M.R., Thudium C.S., Henriksen K., et. al.: Biomarker of extracellular matrix remodelling C1M and proinflammatory cytokine interleukin 6 are related to synovitis and pain in end-stage knee osteoarthritis patients. Pain 2017; 158: pp. 1254-1263.
- Uceyler N., Kafke W., Riediger N., et. al.: Elevated proinflammatory cytokine expression in affected skin in small fiber neuropathy. Neurology 2010; 74: pp. 1806-1813.
- Buchheit T., Van de Ven T., John Hsia H.-L., et. al.: Pain Phenotypes and Associated Clinical Risk Factors Following Traumatic Amputation: Results from Veterans Integrated Pain Evaluation Research (VIPER). Pain Med 2015; 17: pp. 149-161.
- Miller R.E., Miller R.J., Malfait A.-M.: Osteoarthritis joint pain: The cytokine connection. Cytokine 2014; 70: pp. 185-193.
- Kapoor M., Martel-Pelletier J., Lajeunesse D., et. al.: Role of proinflammatory cytokines in the pathophysiology of osteoarthritis. Nat Rev Rheumatol 2011; 7: pp. 33-42.
- Orita S., Koshi T., Mitsuka T., et. al.: Associations between proinflammatory cytokines in the synovial fluid and radiographic grading and pain-related scores in 47 consecutive patients with osteoarthritis of the knee. BMC Musculoskelet Disord 2011; 12:
- Goh L., Samanta A.: A systematic MEDLINE analysis of therapeutic approaches in ankylosing spondylitis. Rheumatol Int 2009; 29: pp. 1123-1135.
- Reed M.R., Taylor A.L.: Tumour necrosis factor inhibitors in ankylosing spondylitis. Intern Med J 2008; 38: pp. 781-789.
- Dogrul A., Gul H., Yesilyurt O., et. al.: Systemic and spinal administration of etanercept, a tumor necrosis factor alpha inhibitor, blocks tactile allodynia in diabetic mice. Acta Diabetol 2011; 48: pp. 135-142.
- Sommer C., Schafers M., Marziniak M., et. al.: Etanercept reduces hyperalgesia in experimental painful neuropathy. J Peripher Nerv Syst 2001; 6: pp. 67-72.
- Arendt-Nielsen L.: Joint pain: More to it than just structural damage?. Pain 2017; 158: pp. S66-S73.
- Wehling P., Moser C., Maixner W.: How does surgery compare with advanced intra-articular therapies in knee osteoarthritis: Current thoughts. Ther Adv Musculoskelet Dis 2016; 8: pp. 72-85.
- Thornton L.M., Andersen B.L., Schuler T.A., et. al.: A psychological intervention reduces inflammatory markers by alleviating depressive symptoms: Secondary analysis of a randomized controlled trial. Psychosom Med 2009; 71: pp. 715-724.
- Chamessian A., Van de Ven T., Buchheit T., et. al.: Differential expression of systemic inflammatory mediators in amputees with chronic residual limb pain. Pain 2017; 158: pp. 68-74.
- Cron D.C., Englesbe M.J., Bolton C.J., et. al.: Preoperative opioid use is independently associated with increased costs and worse outcomes after major abdominal surgery. Ann Surg 2017; 265: pp. 695-701.
- Faour M., Anderson J.T., Ahn N.U., et. al.: Pro- longed preoperative opioid therapy associated with poor return to work rates after single-level cervical fusion for radiculopathy for patients receiving workers’ compensation benefits. Spine (Phila Pa 1976) 2016;
- Tye E.Y., Anderson J., Faour M., et. al.: Prolonged preoperative opioid therapy in patients with degenerative lumbar stenosis in a workers’ compensation setting. Spine (Phila Pa 1976) 2017; 42: pp. E1140-E1146.
- Ben-Ari A., Chansky H., Rozet I.: Preoperative opioid use is associated with early revision after total knee arthroplasty: A study of male patients treated in the veterans’ affairs system. J Bone Joint Surg Am 2017; 99: pp. 1-9.
- Cheah J.W., Sing D.C., McLaughlin D., et. al.: The perioperative effects of chronic preoperative opioid use on shoulder arthroplasty outcomes. J Shoulder Elb Surg 2017; 26: pp. 1908-1914.
- Aasvang E.K., Lunn T.H., Hansen T.B., et. al.: Chronic pre-operative opioid use and acute pain after fast-track total knee arthroplasty. Acta Anaesthesiol Scand 2016; 60: pp. 529-536.
- Villavicencio A.T., Nelson E.L., Kantha V., et. al.: Prediction based on preoperative opioid use of clinical outcomes after transforaminal lumbar interbody fusions. J Neurosurg Spine 2017; 26: pp. 144-149.
- Smith S.R., Bido J., Collins J.E., et. al.: Impact of preoperative opioid use on total knee arthroplasty outcomes. J Bone Joint Surg Am 2017; 99: pp. 803-808.
- Chan F.J., Schwartz A.M., Wong J., et. al.: Use of chronic methadone before total knee arthroplasty. J Arthroplast 2017; 32: pp. 2105-2107.
- Zarling B.J., Yokhana S.S., Herzog D.T., et. al.: Preoperative and postoperative opiate use by the arthroplasty patient. J Arthroplast 2016; 31: pp. 2081-2084.
- Rozell J.C., Courtney P.M., Dattilo J.R., et. al.: Preoperative opiate use independently predicts narcotic consumption and complications after total joint arthroplasty. J Arthroplast 2017; 32: pp. 2658-2662.
- Morris B.J., Laughlin M.S., Elkousy H.A., et. al.: Preoperative opioid use and outcomes after reverse shoulder arthroplasty. J Shoulder Elb Surg 2015; 24: pp. 11-16.
- Morris B.J., Sciascia A.D., Jacobs C.A., et. al.: Preoperative opioid use associated with worse outcomes after anatomic shoulder arthroplasty. J Shoulder Elb Surg 2016; 25: pp. 619-623.
- Menendez M.E., Ring D., Bateman B.T.: Preoperative opioid misuse is associated with increased morbidity and mortality after elective orthopaedic surgery. Clin Orthop Relat Res 2015; 473: pp. 2402-2412.
- Guignard B., Bossard A.E., Coste C., et. al.: Acute opioid tolerance: Remifentanil increases post operative pain and morphine requirement. Anesthesiology 2000; 93: pp. 409-417.
- Mauermann E., Filitz J., Dolder P., et. al.: Does Fentanyl lead to opioid-induced hyperalgesia in healthy volunteers? A double-blind, randomized. Anesthesiology 2016; 124: pp. 453-463.
- Van Gulik L., Ahlers S.J., van de Garde E.M., et. al.: Remifentanil during cardiac surgery is associated with chronic thoracic pain 1 yr after sternotomy. Br J Anaesth 2012; 109: pp. 616-622.
- Nguyen L.C., Sing D.C., Bozic K.J.: Preoperative reduction of opioid use before total joint arthroplasty. J Arthroplast 2016; 31: pp. 282-287. Suppl